Thyroid
Thyroidectomy
Thyroidectomy is a surgical procedure to remove part or all of the thyroid gland. It is performed for various reasons, including thyroid cancer, large goitres, hyperthyroidism (overactive thyroid), and suspicious thyroid nodules.
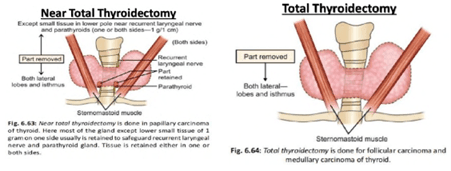
In a Total Thyroidectomy, the entire thyroid gland i.e. both lobes, along with the isthmus, are dissected and removed. This is typically done in cases when a nodule is confirmed to be cancerous on biopsy - especially for papillary and follicular thyroid cancers - to prevent recurrence or spread. Here, the tumour may be greater than 4 cm in size having an obvious extra-thyroid extension or clinically involved lymph nodes, indicating post-surgical radioactive iodine. Other indications for total thyroidectomy are Graves' disease (in cases not responsive to other treatments), and multinodular goitre causing compressive symptoms or other complications.
A Subtotal-Thyroidectomy or Near-Total Thyroidectomy (this is less performed these days) involves removing most of the thyroid gland, leaving a small amount of thyroid tissue behind. It was historically used for Graves' disease, but less common now due to the risk of disease recurrence and complications.
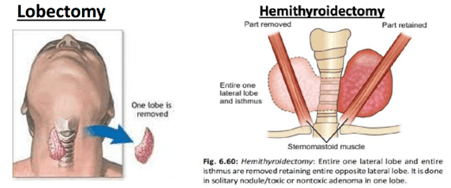
A Lobectomy involves removing a lobe of the thyroid gland. Benign thyroid nodules confined to one lobe, solitary thyroid nodules, or when the diagnosis of thyroid cancer is confined to one lobe without evidence of spread, are some of the indications for this surgery. The size of the nodule is usually less than 4 cm. A Hemithyroidectomy, on the other hand, involves lobectomy and resection of the isthmus (Isthmusectomy). The choice of surgical approach depends on the underlying condition, the extent of disease, and individual patient factors.
Surgical Steps
General anaesthesia is administered to ensure the patient is unconscious and pain-free throughout the procedure. A horizontal or transverse incision is made across the front of the neck, usually along a natural skin crease, to access the thyroid gland. In some cases, a vertical incision may be used. The surgeon carefully identifies and preserves important structures in the neck, such as the recurrent laryngeal nerves (which control the vocal cords) and the parathyroid glands (which regulate calcium levels). After removing the thyroid tissue, the incision is closed with stitches or surgical staples. A drain may be placed temporarily to prevent fluid accumulation. The patient is monitored closely in the recovery room and then in the hospital for any complications.
Recovery
Most patients stay in the hospital for 1-2 days after surgery, depending on the extent of the thyroidectomy and any complications. Patients who undergo total thyroidectomy require lifelong thyroid hormone replacement therapy to maintain normal thyroid function. Regular follow-up visits with endocrinologists and surgeons are necessary to monitor thyroid hormone levels, manage any complications, and assess for recurrence or metastasis in cases of thyroid cancer.
Dr Naveed Basheeth & TOETVA
Thyroidectomy is a well-established procedure with low complication rates when performed by experienced surgeons. Better yet, a more promising alternative is TOETVA (Transoral Endoscopic Thyroidectomy via Vestibular Approach) that comes with many advantages such as truly scar free healing, minimally invasive dissection, and accessible approach to both thyroid lobes.
Dr Naveed Basheeth is a pioneer in minimally invasive thyroid and parathyroid surgery and is also one of very few surgeons in Australasia trained in the TOETVA approach (Police Hospital, Bangkok) for thyroid nodules particularly among the Asian population. His expertise stems from his vast demographic experience in large goitres in the Indian subcontinent population; and complex thyroid cancers in the people of the UK-Ireland, North America, Asia and New Zealand.

